Where to Put It

For the first published version of this article, see “Where to Put It: Tourniquets and Other TacMed TTPs” in the September, 2024 edition of Dillon Precision’s eBlue Press (pages 46 – 48). These images were not with the original article.
*****
The dust was clearing after a gun battle near San Benito, Texas.
Border Patrol Agent Susan Rodriguez lay face down on my left. Her partner Mike, who’d come within inches of getting shot in the ambush, was kneeling next to her, telling Susan to hang on.

Another agent farther off to our left, Ric Salinas, was DRT—shot in the head.

Sheriff’s Corporal (later Lieutenant) Raul Esequiel “Rilo” Rodriguez Sr. (no relation) had been shot multiple times.

One bad guy was down. There were allegedly two more killers still running around. Not knowing where the other bad guys were, we circled the wagons, ramming patrol cars together around where Susan lay. Lesson 1:
If you can’t move a casualty to cover, you may be able to move cover to the casualty.
Cars aren’t exactly cover, but they were better than nothing.
The good guys had plenty of other guns up—mine was just one more—but Mike was not a medic. I was, in the USAF Reserve. I handed my M4 to Deputy “Beaker” Briones, who didn’t have a long gun. Beaker holstered his pistol and covered us with the carbine as I knelt down to assess Susan.
She was bleeding from her mouth and nose. She had a hole about the size of a quarter about 3” off her spine, about halfway down her back. Sucking chest wound, I thought. They taught me what to do about these.
The hole looked like hamburger, but it was not really bleeding much. Covering the exit wound with one hand, I rolled her onto her side. I fished around for the entrance wound, but couldn’t find it.
Needing both hands, I grabbed a different deputy’s hand and pressed it against the hole, then rolled Susan onto her back. I ripped open her green uniform shirt, but couldn’t find the entrance wound. Where the hell is it? I cut open her bra, but still couldn’t see where the bullet went in. I decided to treat what I had already found. I’d look for more problems later.
Today, we would dress an injury penetrating either side of the torso above belly button level with a peel-and-stick vented chest seal.

We had fewer options in ‘98. The deputy’s hand, or the ground, would have to seal the hole in her back, till I could find some plastic and tape to improvise an occlusive (air-tight) dressing. For the time being, Susan had bigger problems. She had stopped breathing.
My CPR facemask was in the Crown Vic, about a hundred meters away from our makeshift bunker. Lesson 2:
If it’s not within arms’ reach when you need it, it might as well be on Mars.
I gave Susan mouth to mouth.
That’s when I spotted the entrance wound. It was in her neck, hiding under her collar. It looked like a small eraser mark, with only a tiny drop of blood sliding out.
The .223 round had hit her spine, damaging three of her vertebrae. It transected a carotid artery, nicked her aorta, and punctured a lung before busting through a rib on its way out.
There was a puddle of blood on the ground, but most of her bleeding had been internal. Unlike ballistic gelatin or blocks of clay, bodies have bone and hollow organs and solid organs and other variations in density and structure. Lesson 3:
There is no way to predict the path a bullet will take in a human.
Deputies stuck Rilo in a cruiser and raced him to the hospital, saving his life. Lesson 4:
With penetrating injuries to the torso, the best medicine is gasoline or diesel. Transport them to a hospital ASAP.
As a NAEMT certified TCCC / TECC instructor, try to I pass on the lessons that Susan and others paid so dearly for us to learn. One of the courses I teach is American College of Surgeons (ACS) Stop the Bleed.
ACS recommends placing a tourniquet a few inches above a wound. Most military programs, in contrast, say to put the tourniquet “High and Tight”—like a Marine’s haircut—as high on the limb as possible.
Why the difference?
*****
ADVANTAGES OF JUST ABOVE THE WOUND
The ACS has good reason for 2” to 3” above. In their world, it makes sense.
A person who has lost a lot of blood needs to safeguard and use what little they have left. The more tissue that is south of that tourniquet, the more of their precious blood is trapped (and leaks out) below it.
If a submarine is hit, leaking air from the forward torpedo room, they don’t close a hatch 1/3 of the way aft, losing all the air (and sailors) in the forward third of the boat. Actually, they would dog all the hatches, so our submarine analogy only goes so far, but you get the idea.
Trauma surgeons rarely see a serious bleed of an arm or leg that has not already been temporarily controlled. If it had not, the patient probably would not have arrived at the ER alive. But let’s say that Guido the Killer Pimp kneecaps Joel right outside the hospital door (if you get that Risky Business reference, you’re probably old like me). When Joel stumbles into the ER, the trauma doc cranks a tourniquet around Joel’s lower thigh, 2 – 3 inches above the wound, just like the ACS recommends.
But Guido’s hypothetical bullet could possibly have bounced off of Joel’s kneecap or the lower end of his femur and traversed the length of Joel’s thigh, just as that real bullet had skidded Susan’s spine. Let’s say it cut the femoral artery 2/3 of the way up the thigh, even though the only blood the doctor can see had leaked out of the hole over Joel’s knee.
The tourniquet is “properly” placed, but Joel’s blood pressure keeps dropping. His breathing is getting faster. His skin is pale, cool and clammy. His thigh is swelling above the tourniquet. Joel’s pulse is rapid but thready, as his heart tries to do its job with less and less blood.
The trauma doc sees the swelling, and changes in Joel’s coloration and condition, in the bright lights of the ER. Knowing one can bleed to death internally into a thigh or abdomen without a single drop of blood hitting the ground, the doctor calls out to the nearest EMT, paramedic, nurse, or janitor: “YOU—hand me one of the other 30 tourniquets in that drawer over there!”
They place the next tourniquet much higher—probably as high as it can go.

*****
HIGH AND TIGHT IN THE FIGHT
Now pretend that you and a wounded friend are hiding behind a car in a dark parking lot, or in a locked closet. You’re slishing around in a puddle of something warm and wet. You rake your friend’s thigh and find a hole in the pants just above the knee. The pants leg is soaked. You’re not sure if the hole you found is the gusher, or if there’s another wound you haven’t found in the dark.

Let’s further assume that you are a responsible, prepared citizen whose EDC, everyday carry, includes a tourniquet.
A tourniquet. Not tourniquetS. Singular.
Are you going to put the only tourniquet you have 2” – 3” above the hole you found, hoping that you didn’t miss another wound in the dark? Of course not. You’re going to place that tourniquet as far up on your friend’s leg as you can—so high up you might have to be careful not to pinch his private parts.
Why?
In that austere environment, with limited resources, that tourniquet must work, the first time. If the tourniquet is high up in the groin, or high enough on an arm to get the patient’s deodorant on it, it will shut off every bleed in that limb.
Say you are sawing wood and you cut your forearm just below the elbow. It’s a real gusher, but the lights are on so you know exactly where the injury is, and you know for a fact there is only one wound. By all means, follow the ACS protocol and place your tourniquet just above the elbow.
If, on the other hand, it’s a gunshot wound (GSW) or you are not sure of the nature and extent of internal injuries (say, a person’s thigh is swelling after a car accident), place the tourniquet High and Tight—as high up on the limb as possible.
NEVER PLACE A TOURNIQUET ON AN ELBOW OR KNEE. Too much bone there; it won’t work. Likewise, cinch around an arm, not over the shoulder.
With a clean amputation, which is rare, 2” to 3” above is fine. In the more likely event of a partial amputation, or if the limb is mangled, say, by being pinched between a motorcycle and a truck or by an explosion, go High and Tight.
Unless you have more tourniquets, avoid placing a tourniquet below an elbow or knee. There are two long bones in each of the forearms and lower legs, and some of the major blood vessels are protected between them. It’s more effective to pinch off blood vessels between a tourniquet and the single bone in the upper arm or leg.
If all of this is too complicated to remember under pressure, just go High and Tight and you won’t kill your patient.
The higher the tourniquet is, the longer it will take the docs to remove it in the hospital. As former Albuquerque PD SWAT sniper Steve Rodriguez likes to tell Thunder Ranch students, that’s “not my problem.”

*****
CONVERSION?
Unless you may be beyond medical help for days (say, your plane crashed on an Alaskan hunting trip, or in the aftermath of a hurricane), NEVER TAKE A TOURNIQUET OFF, OR LOOSEN IT, IN THE PREHOSPITAL SETTING. How and, importantly, when to convert from a tourniquet to another means of bleeding control in a delayed evacuation situation is a study for another article.

Stateside, absent specific training, leave tourniquet conversion to the pros.
*****
TIGHT IS RIGHT
With most tourniquets, like the CAT and SOFT-TW, the magic is in the first pull being as tight as you can possibly get it, before you even begin to tighten the windlass. It must be tight.
When you give blood, they place a restricting band, NOT a tourniquet, on your arm. The restricting band is not tight enough to keep blood from getting into your arm through your pressurized arteries. It is snug enough to reduce venous return to the heart, so the blood backs up and follows the path of least resistance, out the hole they punctured in your vein.

It works the same with bullet holes and knife wounds. If you don’t make the tourniquet so tight it feels like you’re pinching the limb off, you are making the patient bleed out faster.
The first rule of medicine is “Do no harm.” It’s not “Cause no pain.”
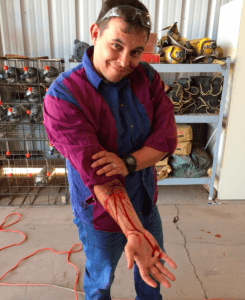
Properly applied tourniquets hurt. If it does not hurt, either your patient is too drunk or high on endorphins to feel pain, or you are doing it wrong.

*****
WHAT IF YOU DON’T HAVE A TOURNIQUET?
The military is getting away from improvising tourniquets. There are ways to do it, but by the time you find the stuff you need, like something long and solid to use as a windlass, your patient may have already bled out. You can pack a hole in a limb just as you must pack a serious bleed in a junctional area (hip, buttocks, shoulder, armpit) that is too high up to tourniquet.

With a partial or complete amputation, you have no choice: if you don’t have a tourniquet, you must improvise one. But wound packing, perhaps in conjunction with an improvised tourniquet like a rigger’s belt, should keep a patient with a GSW or knife wound to a limb alive.

