BVMs

A Bag-Valve-Mask, or BVM, is a device for giving Rescue Breaths, consisting a squeezable, semi-rigid bag, a facemask, and a one-way valve. BVMs do not require that you get your face into the other person’s face area, reducing the risk of disease transmission.
BVMs allow us to put a higher concentration of oxygen into the patient. If you are giving mouth to mouth (something we officially discourage, unless it’s at least through a shield), or mouth to mask, your exhaled air only contains about 14% oxygen. If you are using a BVM with room air, your patient will be getting 20% O2 or more. If you hook a BVM with a reservoir to an oxygen source, you patient will be getting up to 100% O2.
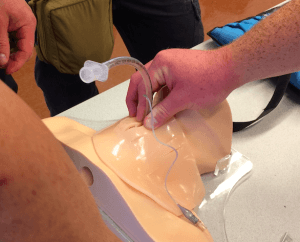
BVMs are awesome tools, but they require specific hands-on training. Overzealous application of a BVM hooked directly to an Endotracheal Tube or even an Esophageal Airway can very easily kill your patient, by pumping so much air into their chest that blood has a difficult time returning to their heart to be pumped out into circulation (either by the heart itself, or by a rescuer squeezing the heart during CPR). The only advantage of hooking a BVM up to a definitive airway is that rescuers pumping on the chest do not need to interrupt compressing the heart for you to give a breath. Instead, just gently squeeze the bag every 6 seconds or so.
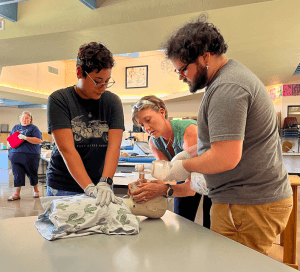
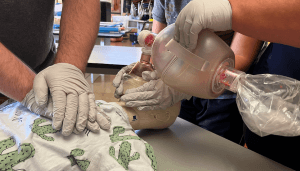
One of the most difficult parts of using a BVM is establishing a proper seal of the mask to the patient’s face. Blowing air on their cheeks will not save them. You must put the air in their lungs, and that requires a fairly hermetic seal. Common errors include pushing the mask onto the patient’s face, rather than pulling the casualty’s face up into the mask while opening their Airway. Hook your fingers under the back angle of the jaw and pull up.

Pull the face up into the mask by hooking your fingers under the angle of the jaw and pulling up. Use the entire side of your thumbs, from the last knuckle to the thumb side of the palm, to hold the mask snugly against the patient’s face. There’s no bag on this “BVM” so you can see how to establish the seal.

BVMs can be operated by one very well trained person, but they work best when one person maintains the seal and another squeezes the bag.
Another common error when using a BVM in conjunction with a definitive airway (like an ET tube) is squeezing the bag too fast.
That used to be a thing. When I was working in the Emergency Room at Scott Regional Medical Center in 1992, it was an officially accepted technique we called “hyperventilation.” The erroneous idea was to get as much oxygen in there as possible. Instead, we wound up filling up the patient’s chest with so much air, blood could not return to the heart, as described above.
If the patient is in a medically induced coma, or you are pumping air into them via an ET tube during CPR, simply squeeze the bag, slowly, every six seconds. If you are using a BVM with a facemask during CPR, squeeze twice after every 30 compressions.
The final foibles associated with BVMs have to do with access. It’s easy to carry a small folding face shield on your keychain, and if you are really prepared you could carry a “hard” CPR face mask in a cargo pocket. But BVMs don’t travel well on your person. If left in your car in the summer, the soft pliable plastic of a BVM can dry out, melt, stick to itself, or deform. They tend to get crushed under other stuff in soft-sided portable med kits.
Even if you do have access to a BVM, it might be the wrong size–say, an adult sized bag and mask when your patient is a toddler. There are workarounds, such as putting the mask on upside down and squeezing the adult bag with only your thumb and forefinger, but such improvisations are an inexact science, fraught with difficulty for the rescuer and hazardous for the patient. An Adult-sized BVM can be pressed into service for anybody, but if you can afford kids’ sizes, you should get some. At least have one that will fit the age ranges in your environment.

Opioids Don’t Kill People
Opioids tell your body not to breathe. Not breathing kills people.
Even if you have Narcan (Naloxone), your OD patient will need aggressive ventilatory support before and after you administer it, if they are to survive (aggressive ventilations are also important for kids who fall into pools). Since addicts will do anything–anything–to get their next fix, you probably don’t want to be locking lips with anybody who ODs. Even in the post-COVID era, you probably don’t want to get your face anywhere near theirs.
If you are trained and equipped to use them, BVMs are great lifesaving tools.
–George H, Heloderma Medical

